Sterile manufacturing environments are open to many sources of potential contamination if not managed correctly. Air filtration systems, materials transfer and operators all pose potential risks – a fully gowned operator may create as many as 150,000 particles per minute, many of which are viable and potential hazards during the manufacture of sterile drugs. The need to ensure the safe and sterile transfer of active pharmaceutical ingredients (APIs) and other formulation ingredients during aseptic processing has driven the development of multiple techniques that can be employed in cleanroom environments.
Approaches to aseptic manufacturing
Barrier technologies such as isolators and restricted access barrier systems (RABS) are designed to provide micro-environments which have been seen to offer better levels of microbiological protection for a process than traditional open cleanroom environments. The aim is to separate the operator from the product and prevent harmful contamination spreading to critical operations in the drug production process.
Isolators provide an enclosed working space that is detached from the surrounding environment, enabling manipulation to be undertaken within the enclosure without compromising integrity of the space. High Efficiency Particulate Air (HEPA) filtered air is supplied to the chamber in a laminar flow to ensure particulate generation is suppressed and removed efficiently. The integrated bio-decontamination system ensures a validated 6 log reduction to the transfer process.
Due to the high-performance requirements for these enclosures, integrated pressure decay tests have become the norm during start up and prior to any bio- decontamination phase, with the leak of the chamber being a key factor in the classification of the device. See ISO14644 on leak rates for separative devices.
As an alternative to the Isolator approach RABs (Restricted Access Barrier Systems) offer various levels of barrier protection with both open / closed and active / passive systems. Their integrity is generally accepted as less than that of an Isolator so RABs must be set-up in higher-class environments, generally grade B cleanrooms.
RABS contribute distinct advantages by enabling operators to maintain a distance from the process, while allowing the operational flexibility for the enclosure to be opened if significant intervention is required. In comparison to isolators, RABS can ensure faster start-up times and improve the ease of product changeover. They can also reduce validation expenditure.
Even with barrier separation there is still interaction. One of the greatest areas of concern for both Isolators and RABs is the transfer of materials into or out of the enclosure. There are a number of methods employed for achieving this interaction although many are finding that the use of aseptic split butterfly valve (SBV) technology, a direct transfer device, being the most user friendly and robust solution.
SBV technology
The aseptic SBV provides a safe method of transferring product from one container, process vessel, isolator or RABS to another, while ensuring the sterility of the transfer is not compromised.
Fundamentally the SBV consists of two halves, the active (Alpha) unit and the passive (Beta) unit. Each half consists of half of the ‘butterfly’ disc. The active unit is attached to the stationary process equipment such as a mixing vessel, while the passive unit is attached to the mobile container such as an intermediate bulk container (IBC) or flexible bag. When the two parts are brought together, the disc halves join to form a single disc, sealing exposed any surfaces. The two discs then operate as one disc and can be opened to allow transfer of product from one location to another.
SBV can contribute considerable cost savings in comparison to traditional approaches, being as much as three to five times cheaper than alternative methods. The aseptic SBV also makes it possible to downgrade the surrounding cleanroom environment because of the integrity of the solution.
Adoption of aseptic SBV technology allows manufacturers to benefit from a closed handling method that not only achieves the required sterility assurance level (SAL) and reduces the requirement for manual intervention, but also offers the opportunity to reduce the resource associated with cleaning and validating large areas. By minimizing cleaning requirements, SBVs limit downtime, while also increasing flow and yield from product transfers.
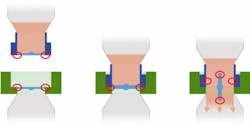
FIGURE 1
Eliminating the ring of concern
The area of concern exists within the small area where the outer circumferences of the disc interfaces (that are exposed to the room environment) seal together and rotate into the open critical area. (As shown in Figure 1.)
This is known as the “ring of concern” and is common in any aseptic transfer device. Effective techniques must be used to remove the risk of contamination impacting the sterility of the disc surfaces.
Traditionally, SBVs uses vaporized hydrogen peroxide (H2O2) gas to bio-decontaminate and remove contamination on the two mating surfaces of the valve before the product is transferred. The two halves of the valve create a sealed chamber by partially docking the two-disc faces, allowing a decontamination to take place in a closed environment. This prevents further contamination from taking place after the decontamination process is finished, unlike the traditional sporicidal spray and wipe approach, which is generally carried out in an unsealed environment therefore allowing contamination to occur.
Previous research, such as that of M. Sawyer et al. in 2014, lists the differences between the two types of bio-decontamination media in terms of a typical cycle, however SBV technology with chlorine dioxide (CD) gas had not been evaluated. For any technology to be adopted within a validated production process, qualification evidence should exist to prove the technology prior to live process validation.
In this example, qualification testing was carried out by SBV manufacturer ChargePoint Technology and Clordisys Solutions, which provides decontamination services utilizing CD gas.
To provide optimal sterility assurance, the SBV must prove to bring about a 6 log (10-6) reduction in microbiological contamination on the surface areas of the device exposed to the decontamination cycle. Typically, this reduction is validated with the use of a biological indicator (BI) and subsequent controlled laboratory analysis of bacteria culture growth.
A cycle development and optimization study was performed to test the feasibility of CD gas to sterilize the mating surfaces to the required SAL and to perform such cycles in as short a time as possible. The study determined the compatibility of materials in contact with the CD gas, and also examined how pressure may or may not cause leaks in the system.
Cycle development and optimization methodology
FIGURE 2: In the experimental setup, chlorine dioxide gas flowed into the assembly from the right for (n) seconds and then the ball valve on the left was closed.
All the testing was done with CD gas generated by Clordisys’ Minidox-M CD Gas Generator. CD gas was injected manually from the Minidox-M (see Figure 2) and allowed to flow for (n) seconds through the valve assembly. The outlet valve was then closed, after which the Minidox-M valve was closed. A high concentration of CD gas (100 mg/L) was then trapped in the valve assembly.
Parameters and operation
Clordisys approaches every gaseous decontamination effort as if it were to obtain a 6-log sporicidal reduction. Reducing spore counts is more difficult than reducing viruses and other organisms. Sporicidal reduction also requires humidity to soften the spore walls to enable the gas to penetrate and kill the microbes.
The CD decontamination process consists of the following steps:
• humidification to soften the spore walls
• introduction of CD gas to reach the desired concentration
• a dwell period (i.e., exposure to the gas) in which the gas sits for a period of time to obtain the desired kill level
• aeration to remove the gas.
The humidification range required to soften the spore walls is at least 60 percent, with an optimal level of 65–70 percent. Lower relative humidity levels require longer exposure times or more dosage. The exposure level and time that Clordisys targets to obtain a 6-log sporicidal reduction is 1 mg/L (360 ppm) at two hours. This equates to 720 ppm-hours of dosage. Clordisys has demonstrated 6-log sporicidal reduction as low as 450 ppm-hours. At the end of exposure, the gas is aerated until the concentration drops to 0.1 ppm, which is the 8-hour safety level as well as the odor threshold level.
In this application, the concentration levels of CD used were reduced, compared to a typical cycle taking place in a large room. This was due to the small size of the chamber once the valves were closed.
A first set of experiments were performed with a fixed time gas flow. The system was connected as shown in Figure 3 with the 1/4” ball valve open to the scrubber and one BI placed in the valve assembly. The Minidox-M outlet valve was manually opened and gas flowed to the scrubber for 20 seconds at 20 liters per minute (LPM). The ¼” ball valve was then closed, followed by the Minidox-M outlet valve. The BI was then tested with multiple exposure times of 1, 2, 5, and 10 minutes. Each exposure time cycle was repeated three times for three cycles, for a total of 12 cycles with 12 BIs.
At the end of each exposure (1, 2, 5, and 10 minutes) the Minidox-M sample pump was energized and the ¼” ball valve was opened to blow the CD gas to the scrubber. The aeration time required to bring the CD gas to below detectable levels was two minutes.
A second set of experiments was performed with a fixed time gas flow using the same system connection and experiment times, but the gas flowed to the scrubber for 60 seconds at 20 LPM.
A third set of experiments was performed with an exposure time gas flow. The system was connected in the same way with the ¼” ball valve open to the scrubber and one BI placed in the valve assembly. The Minidox-M outlet valve was manually opened and gas flowed to the scrubber for 20 seconds at 20 LPM. The ¼” ball valve was not closed, however, and gas was allowed to flow for the entire exposure time. Exposure time started after 20 seconds of flow.
The BI was then tested with the same exposure times and number of cycles as in the first experiment. At the end of exposure (1, 2, 5, and 10 minutes) the Minidox-M sample pump was energized and the ¼” ball valve was opened to blow the CD gas to the scrubber. In this case, the aeration time required to bring the CD gas to below detectable levels, was also two minutes.
A fourth set of experiments was performed with a fixed time gas flow and pressure build up in the valve assembly. For these cycles, the system was connected as shown in Figure 3 with the ¼” ball valve open to the scrubber and one BI placed in the valve assembly. The Minidox-M outlet valve was manually opened and gas flowed to the scrubber for 20 seconds at 20 LPM. The ¼” ball valve was then closed. The Minidox-M outlet valve was closed after pressure increased to 10 psi (68.9 KPa). The BI was then tested with the same exposure times and number of cycles as in the first experiment. At the end of exposure (1, 2, 5, and 10 minutes) the Minidox-M sample pump was energized and the ¼” ball valve was opened to blow the CD gas to the scrubber. Again, the aeration time required to bring the CD gas to below detectable levels was 2 minutes.
Results
Cycle times for the four sets of cycles varied due to the exposure time and gas flow time. The shortest cycle was 3.3 minutes and the longest was 13 minutes. The shortest successful cycle (defined as three runs with no positive BIs was 7.3 minutes). This is extremely fast when compared to a conventional airlock or isolator which could be in the region of four to six hours. CD gas can be used as an alternative to H202 vapor for decontamination.
Table I shows the cycle data BI results. In each run, only one BI was placed in the valve assembly. Room relative humidity during the cycles was 30–40 percent.In the pressure-hold test (the fourth set of tests), when the pressure within the assembly was raised, a low-level CD gas sensor was used to measure any leakage on both sides of the valve assembly for the entire exposure time. No leaks were detected on either side.
No material effects (e.g., degradation/cracking) were noticed after all testing was performed. The valve underwent a minimum of 48 cycles at 100 mg/L CD gas concentration. The total dosage for all cycles was approximately 130,000 ppm-hrs. This total dosage is equivalent to 180 runs at a normal room concentration of 1mg/L.
Conclusion
The purpose of the test was to ensure that a 6 log (10-6) reduction in microbiological contamination was achieved on the exposed faces of the valve. This result was achieved on all 5- and 10-minute cycles. No biological growth was seen in any of the BIs in these cycles. The cycle times presented consistent bio-decontamination at five minutes, which is faster and more consistent than was found in previous tests of H2O2 cycles.
During the leak rate analysis, in which the gassing space was pressurised and low-level readings were taken above and below the discs, no levels of gas detection were found. Considering that CD is a pure gas and therefore inherently easier to detect than H2O2 vapor, the results proved the process to be a robust solution that can be safely used with both CD and H2O2 vapor.
In the future, it would be beneficial to test the system with longer pipe runs to ensure that the fast aeration times can be maintained. Longer pipes would allow drug manufacturers to house the generator in one location within the facility and the valve in the process area without the concern of prolonged cycle times.
Final thought
The selection of an appropriate aseptic transfer technology will come down to a variety of factors, including the unique requirements and possibilities within a manufacturing facility, as well as the type of products being processed. Isolators are easier to decontaminate, monitor and offer a high degree of sterility assurance, while RABS provide both increased operational flexibility and speed of changeover which appeals to many manufacturers, particularly contract manufacturers that need to be able to adapt to different customer products and manufacturing processes.
Aseptic SBV technology not only complements and works in harmony with these solutions but in some applications, can also replace them. Reducing the reliance on cleanroom environments, they also offer increased sterility assurance and improved ergonomics. Barrier systems are vital to ensure product quality and operator protection, and each of these technologies has its place. It is vital that a full evaluation of products and processes against the various systems takes place in an early project phase to ensure the right technology is selected.
References
1. M. Sawyer et al., “Got Gas? Chlorine Dioxide or Vaporized Hydrogen Peroxide: Which one is right for you?”, Poster Presentation, Biosecurity Research Institute, Kansas State University, 2014, www.absaconference.org/pdf55/003Sawyer.pdf